Tecvayli Effective in BCMA-Pretreated R/R Multiple Myeloma
Tecvayli responses were found to be slightly lower in patients with relapsed/refractory myeloma treated with another BCMA-targeted therapy.
Patients should have discussions about Tecvayli as treatment after previous BCMA-directed therapy with their doctors, an expert said.
Treatment with Tecvayli (teclistamab) may still be an effective option for patients with relapsed/refractory multiple myeloma who have previously received anti-BCMA therapies. However, this patient population may be slightly less likely to respond to the treatment, according to research published in Blood Advances.
In a real-world study (conducted outside of a clinical trial setting) of 47 evaluable patients who received Tecvayli, the objective response rate (ORR; patients who responded partially or completely to treatment) was 64%, with 38% achieving a very good response (90% or more decrease in a myeloma-associated protein in the urine) or better. ORR was 50% among patients who received previous BCMA therapy.
At a median follow-up of 3.1 months, median progression-free survival (PFS; the time a patient lives without their disease spreading or worsening) was not reached for the full patient population or in the BCMA-naïve subgroup, meaning less than half of the patients’ diseases had progressed. But PFS was 3.4 months among those who received prior BCMA therapy.
Dr. Ross Firestone, one of the co-authors of the study and a hematology oncology fellow at Memorial Sloan Kettering Cancer Center (MSK) in New York, discussed the study, its findings and its significance as a work of real-world research.
What were you and your colleagues were hoping to learn with this study?
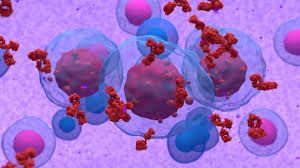
At the time this study was first done, [Tecvayli (teclistamab)] had just come onto the market. It's part of a group of therapies for multiple myeloma called bispecific antibodies, and [Tecvayli] was the first bispecific antibody for multiple myeloma that got [Food and Drug Administration (FDA)] approval.
[Tecvayli] works by redirecting the energy of a patient's immune system towards fighting multiple myeloma cells. It is able to recognize multiple myeloma cells by targeting a protein that's on the multiple myeloma cells called BCMA.
Now, a number of other therapies for multiple myeloma also go after that same feature of myeloma cells, that BCMA target. And we wanted to know if people who had had drugs that have targeted that same thing in the past could still benefit from [Tecvayli]. Because sometimes, therapies that go after BCMA stop working when the cancer cells change the BCMA target in some way. So, we were wondering if there was a possibility that patients who had had those drugs before wouldn't be able to use [Tecvayli] well, because their myeloma had already adapted to those older therapies.
Can you explain the findings?
The first thing that we wanted to do is look at at, from a clinical perspective, how well [Tecvayli] patients did, and if there was any difference in the people who had gotten something targeting [BCMA] before versus the people who hadn't. What we saw was the people who had gotten something targeting [the BCMA protein] before did a little bit worse. Not quite as many responded, but they still did very well in terms of where they were with their disease, and with respect to other therapy options that they would have had.
What we wanted to do is try to figure out why the therapy failed certain patients, and why it worked out for other patients. We looked specifically at that target protein, BCMA, to see if it was compromised in some way. And we found that in the overwhelming majority of patients, it was fine, there was no problem.
This was a real-world study, as opposed to a clinical trial. Can you tell me about those two different ways of looking at patient outcomes and why real-world data such as this is particularly valuable?
This is actually especially important for this study. When patients are enrolled in clinical trials, they're either receiving an experimental therapy or a therapy that's been thoroughly tested but it's being looked at in a new way.
In a real-world study, [there are] a lot of patients who wouldn't have otherwise been eligible for the clinical trial, because they might not be the ideal candidate the trial’s looking for. Those patients can now get the medicine to see if the drug works as well when you're not looking at this optimal scenario.
But what's interesting about this drug [Tecvayli] specifically is that one of the exclusion criteria for the original clinical trials, so one of the reasons why patients wouldn't be allowed to enroll, is if they had therapies targeting that BCMA protein in the past. So, our study was really the first study to show this therapy in patients who had had those therapies in the past. And we see that therapy still works very well.
Given these findings, what sorts of conversations should patients be having with their doctors?
I think there are a few, some of them relate to a follow-up study that we've done, where we can actually look at that BCMA protein before we choose what therapy people get. In that sense, a conversation that some people will have with their doctor is whether they should be tested for that at all — and if they do get the test, what that test means, and whether it means they should go ahead with a drug like [Tecvayli] or switch to something else.
The other conversation that's relevant is that even if someone's had a BCMA-directed therapy in the past, this data may assist in discussing why it might still make sense to go with [Tecvayli], which works very similarly to those other drugs, even though those other drugs either didn't work at all for them or were working but stopped working at a certain point.
One thing that we also found in this study is that one of the really common side effects that a lot of patients are concerned about with regards to this therapy is something called cytokine release syndrome, which is a side effect that we see frequently in patients who get this drug. But what we found is that the patients who have that side effect actually all responded to the therapy. So, it's actually an indicator that the therapy is working, even though it might be tough for the patient at the time they have it. So if patients are worried about cytokine release syndrome, doctors can discuss with their patients how they may have already planned what to do and how to manage it if it happens, but also that it's probably a good thing if it happens as opposed to a bad thing.
Transcript has been edited for clarity and conciseness.
Interested in the latest research and information in multiple myeloma care? Register for Educated Patient® Multiple Myeloma Summit!
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.