Metastatic Breast Cancer Treatment is ‘Not One-Size-Fits-All’
A metastatic breast cancer diagnosis can come as “a shock,” but experts spoke with CURE® about ways patients can navigate their experiences and treatments.
Having a professional support system can be important after receiving a diagnosis of metastatic breast cancer.
Receiving a diagnosis of metastatic breast cancer “usually is a shock” for patients and their families, an expert told CURE®. However, there are steps patients can take, and conversations they can have with care teams that make the process easier to navigate.
“I usually consider day one in the clinic as the most important visit with patients,” Dr. Maria Hafez said. “We need to be very honest, give accurate information, as well as [being] detailed and thorough about what treatment management we have, and also, survival and prognosis.
Hafez is a medical oncologist and director of clinical breast cancer research at Jefferson Health.
“After this talk with the oncologist and receive the pathology or the diagnosis of having metastatic breast cancer, … I will say, [manyof my] patients will feel way better.”
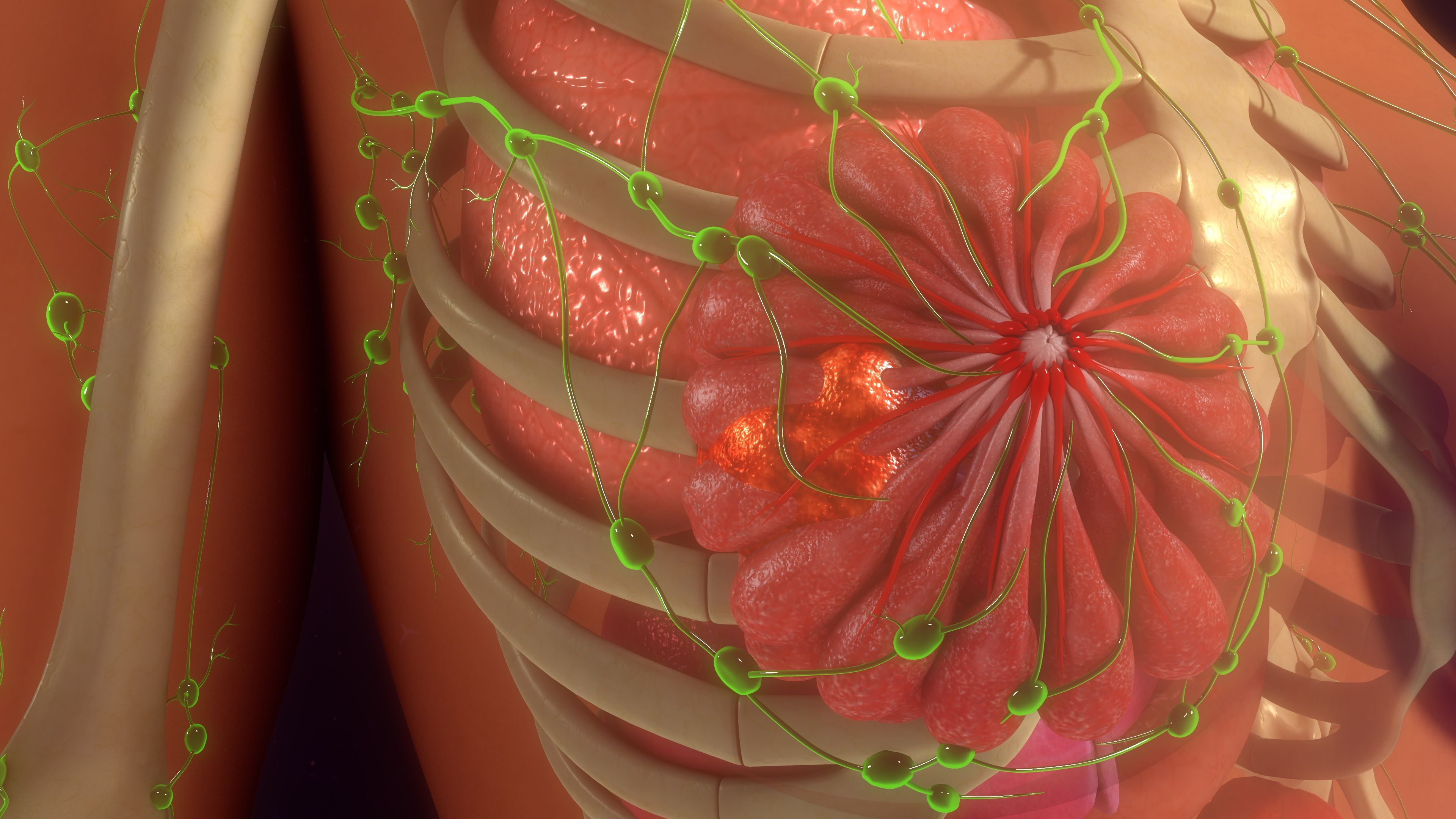
Metastatic breast cancer — according to Penn Medicine — is when the cancer has spread (metastasized) to other organs or lymph nodes away from the breast.
“I've heard some analogies [that metastatic breast cancer is] like a dandelion, so it like blows the seeds and it gets spread everywhere,” explained Krissa Smith. “So the primary tumor makes one big ball of cells, but with metastasis, it spreads around [like] seeds throughout your body.”
Smith is the vice president of education at Susan G. Komen, a nonprofit organization that funds research and provides resources for patients with breast cancer.
“What we've learned over years, [after] more than 40 to 50 years of research, is that breast cancer is not one-size-fits-all,” Smith explained. “We started out thinking all breast cancers were the same. And every year we learn more about how it's very unique to the individual.”
READ MORE: Tailored Treatment for Breast Cancer
Treatment Options for Metastatic Breast Cancer
There is currently no cure for metastatic breast cancer, although it is treatable, Smith said.
When the breast cancer metastasizes to certain areas, such as the lungs, brain or bones, Smith explained that the treatment is going to be different than typical treatment.
“That really gets to where we're trying to go with precision medicine and being able to treat your tumor, your metastases and making sure that it's going to be the best for you not only, from an effectiveness perspective, but also for side effects and the ability to stay on treatment and having the right access,” she said.
Hafez also noted that routine scans to ensure patients are responding to treatment is important.
“However, given that we're going to do the treatment, we usually have to monitor the treatment by doing imaging every three months to make sure that patients are responding to treatment,” Hafez said.
She emphasized that treatment should not be intolerable, and that the scans indicate if the cancer is responding to the treatment.
“We need to remind patients and ourselves as oncologists: we are not treating a cancer we are treating patients,” Hafez said. “So that's very important to not just follow the guidelines, but also what my patients’ performance statuses are, toxicities, side effects, all these things and then tailor the treatment multiple times.”
‘I Was Told I Was Cured.’
Staying up to date with the latest treatments was deemed beneficial for Pam Kohl, who originally received a lumpectomy, radiation and endocrine therapy. At age 58, she received a diagnosis of early-stage breast cancer after an annual mammogram, she said during an interview with CURE®.
“At the end of the endocrine therapy, I was told I was cured,” she said. “And that I could look breast cancer in my rear-view mirror, that it was done.”
Three years later, her annual mammogram showed something “suspicious,” Kohl noted. After some scans and tests, her care team insisted that nothing was wrong. However, a biopsy showed that she likely had a recurrence of estrogen-positive breast cancer.
Kohl advocated for a positron emission tomography (PET) scan but was told it was unnecessary because it was “just a recurrence.”
A PET scan is a certain type of imaging that shows pathways that may show signs of cancer spreading, according to the Cleveland Clinic. Other scans, such as a mammogram and ultrasound did not pick up on the disease spread, Kohl noted.
After pressing for the PET scan, Kohl finally received it and determined that she had metastatic breast cancer after two areas lit up in the lymph nodes near her lungs.
Kohl explained that she currently takes an oral treatment to help maintain her metastatic breast cancer and is aware of acute reactions to treatments. She said she received scans every three months to monitor her responses to treatment, but her anxiety around scans (scanxiety) is still present.
“I’ve gotten scanned every three months for seven years. And dealing with just the scanxiety alone, much less the results of those scans, [can be overwhelming],” she said.
Tips for Patients and Their Families/Caregivers
The time after receiving a diagnosis for metastatic breast cancer can be “turbulent,” Smith noted, which is why finding a professional support system can be important.
Working with a patient navigator is a way to relieve some of the stress that comes with decision making, she said.
“There's a lot of decision fatigue that happens. And for those who have limited resources, or who just don't know how to navigate the system, … things [can] get delayed,” Smith explained. “So having someone, [such as a patient navigator], who can go with you and support you, is amazing.”
It’s also important for family members or caregivers to understand what a patient needs, said Dr. Casey Degen, a medical oncologist, director of clinical research and the breast lead at Jefferson Health Northeast.
“It's really important for caregivers to realize what the patient needs and be there, even if the patient can't necessarily explain what they need,” Degen said. “But also, really communicate with the oncology team, the physician and with the nursing and infusion staff. We're getting better at offsetting the effects of chemotherapy or of anti-cancer treatment, and we can do that as long as we know what's going on. So just really having open lines of communication is helpful.”
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.
A Patient With Breast Cancer Explains How Her Job Saved Her Life
October 13th 2022A woman with stage 2 invasive ductal carcinoma — a type of breast cancer that begins in the milk ducts of the breast — shares how her experience as an employee at a breast cancer research facility helped her push against doctors who minimized her ultrasound findings and how her Ki-67 score informed her treatment choices.
Listen
Katie Couric and Paula Schneider: Sharing Cancer Journeys One Letter At a Time
October 29th 2020In this episode of the “CURE Talks Cancer” podcast, we spoke with television journalist Katie Couric and Susan G. Komen CEO Paula Schneider about their experiences with cancer, and the advice they offered their pre-cancer selves.
Listen