It Takes a Village: Cancer Caregivers Need to Care for Themselves, Too
Caregivers of patients with cancer may face financial toxicity and stress — with little time to take care of themselves.
For Danna Wessels of Austin, Texas, it all began with two itchy patches of skin on her abdomen. In 2007, Wessels, now 63, received a diagnosis of stage 1a mycosis fungoides, a form of cutaneous T-cell lymphoma.
At the time, her then-partner and now wife of nine years, Nancy Noble, made one request: “I asked her not to look at the (internet) when she got the diagnosis,” Noble says. “Because I did.”
Nancy Noble (left) took three weeks off work, along with picking up other caregiving responsibilities, after her wife, Danna Wessels received a diagnosis of a rare type of lymphoma.

Their lives changed quickly as Wessels faced constant itchiness that made normalcy a challenge. “Danna couldn’t really go out,” Noble says. “I felt pretty helpless.” Still, Wessels, who also has
type 1 diabetes and Addison’s disease (an autoimmune disease in which the body attacks the adrenal glands and destroys them), was no stranger to managing chronic medical conditions. But Noble knew from her research that things could get worse — and they did.
The disease moved from Wessels’ skin to her blood, and in June 2011, she required a stem cell transplant. To prepare, Wessels had 40 treatments of total skin electron beam therapy, a type of radiation that treats the skin on the entire body, over 10 weeks. After her stem cell transplant, she remained in the hospital for 28 days.
Noble worked from her wife’s hospital room and then took three weeks off from her high-pressure job at a medical device company to care for her. “She was amazing,” Wessels says. “She was my rock. She did it all.”
"She was amazing. She was my rock. She did it all," Dana Wessels said.

“All” included learning how to flush the port in her wife’s chest with sterile fluid to keep it clean. It also included nonstop housecleaning to help prevent infection and preparing food to help Wessels build her strength. When she had to return to work, Noble hired outside help to care for her wife during the day and drive her to appointments.
A blood cancer diagnosis a loved one is frightening, Noble says. “I knew there was only so much I could personally do,” she notes. Instead, she focused on the practical details and relied on her faith that things would work out. “It’s one of those experiences where I say, ‘How did we do that?’” Noble says. “I just remember doing what we had to do.”
Noble knew taking care of herself was critical. “I lost about 30 pounds in preparation for Danna’s transplant because the last thing you need is to get sick yourself,” she says, adding that as the provider of the family’s insurance, she worried about job security. “I told management, ‘This is what’s going on, and it’s a big deal.’ Fortunately, they were sympathetic.”
Reality of Caregiving
Wessels says Noble took on another important caregiving role: keeper of information. She spoke with doctors and managed details so Wessels didn’t have to. But for some caregivers, managing those details and participating in the decision-making process can feel overwhelming.
Having a good understanding of disease prognosis can prove critical. Yet sometimes caregivers may not be clear on what they’re being told or may have trouble accepting it. A study presented at the 2021 annual meeting of the American Society of Clinical Oncology found that some caregivers don’t acknowledge that their loved one is terminally ill.
Study author Dr. Elizabeth O’Donnell, director of lifestyle medicine and a medical oncologist in the Multiple Myeloma Disease Center at Massachusetts General Cancer Center in Boston, and her colleagues studied 127 caregivers of patients with multiple myeloma in various treatment stages. They found that although more than 80% of caregivers understood the oncologist’s message that multiple myeloma is an incurable cancer, only 53% said their loved one was incurable.
Although physicians do a good job of telling patients and caregivers about prognoses, caregivers often leave “space for hope,” O’Donnell says. Still, understanding prognosis plays an important role in how caregivers cope. In O’Donnell’s study, more than 88% said it was extremely helpful for coping.
“Within our blood cancer population, particularly with multiple myeloma, where you have an incurable but long-term illness, levels of stress and distress can be quite high for most patient caregivers,” she says, adding that that’s why having support is critical for caregivers.
Sarah Miretti Cassidy, director of external affairs for the Chester, New Jersey-based Cancer Hope Network, knows exactly how important support is. The organization trains cancer survivors and caregivers as support volunteers and matches them with clients currently undergoing treatment or caring for a loved one with the disease. Cassidy, herself, was matched with a caregiver volunteer when she was caring for her mother-in-law.
“Connecting with a volunteer helps you know that you’re not alone,” she says. “That’s probably the biggest benefit that Cancer Hope Network offers to caregivers. It may be the first time you’re caring for a loved one, but you’re not the first person who is caring for a loved one.”
Her volunteer helped with practical information such as what to expect when chemotherapy started and a helpful method for moving her mother-in-law without hurting her, Cassidy says.
“Volunteers don’t tell you what you should do,” she says. “They share their experience and offer suggestions. They say, ‘Here’s what worked.’”
Patricia Hlafter had experience caregiving prior to her husband’s diagnosis of hairy cell leukemia.
Patricia Hlafter of Princeton, New Jersey, volunteers with the organization to help support other caregivers. She cared for her husband, who has been treated for what she calls a “very treatable” hairy cell leukemia. “He did pretty well,” Hlafter says, noting that he had a busy job at the time, so in her role as a caregiver, she had to make sure he ate and took care of himself.
But Hlafter also cared for her mother, who had stage 4 non-Hodgkin lymphoma and died in 2000.
That experience was very different from caring for her husband, she says, adding that she shared caregiving responsibilities with her two sisters.
Hlafter scaled back her work so she could drive her mother to chemotherapy appointments, and the two would chat during her treatments. “One of the benefits was the opportunity to have all that time with her,” she says.
When cancer ultimately returned, Hlafter’s mother decided to forgo a third round of chemotherapy. “That made me sad,” she says. “But I knew there was no choice except to respect her decision.”
Now, Hlafter helps caregivers strategize about how to care for their loved one and themselves. “I think that when someone is a caregiver for the first time, you don’t know what the rules are,” she says. “You have to know that you will make mistakes, and you have to follow your instincts.”
Communication Is Key
Listening is critical, Hlafter says. She encourages caregivers to talk with their loved one about how they’re feeling. When caregivers pay attention to those everyday conversations, they can learn a lot, she says. “Be alert for the clues your patient gives you,” Hlafter adds. “It helps you to help them.”
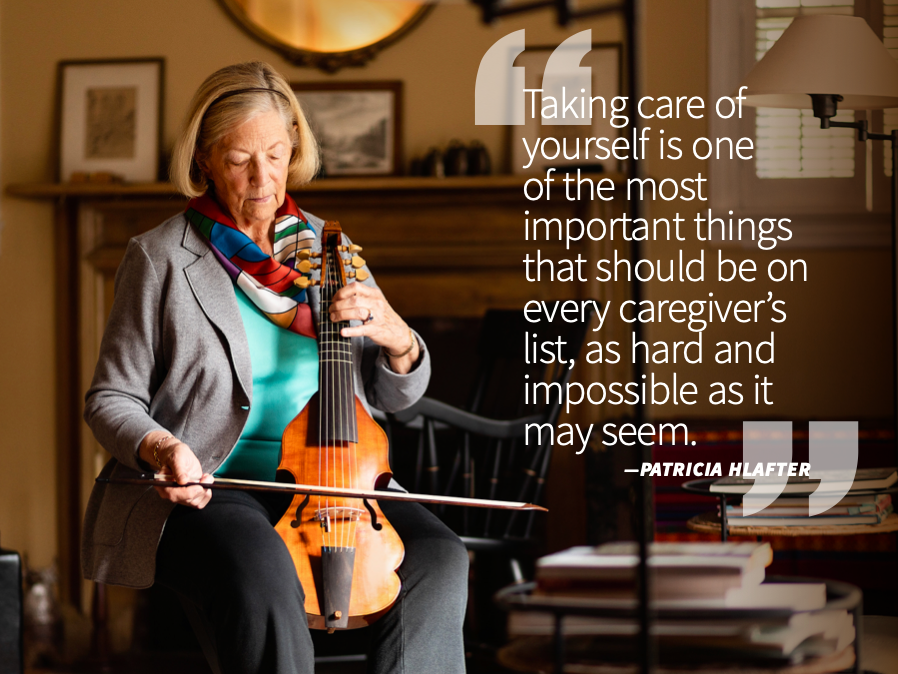
"Taking care of yourself is one of the most important things that should be on every caregiver’s list, as hard and impossible as it may seem." — Patricia Hlafter
It’s also important for caregivers to know as much as possible about the patient’s illness. “The more you know, the more you’ll understand some of the things that might happen during the course of treatment,” she emphasizes. “It helps you know what’s normal for someone who is undergoing cancer treatment and what is alarming and needs to be brought to the attention of the doctor immediately.”
Getting needed information can be challenging for some caregivers, according to Carma Bylund, a professor in the department of health outcomes and biomedical informatics in the College of Medicine at the University of Florida in Gainesville. Bylund and her colleague Carla Fisher, have partnered with the Leukemia & Lymphoma Society to study caregivers of people with blood cancer. Their most recent study, which was published in the May 2021 issue of Translational Behavioral Medicine, examined the effects of COVID-19 on adult caregivers of parents with blood cancer. But some of the themes that emerged are applicable to all caregivers — particularly those around communication, Bylund says.
“We’re seeing more attention being paid to what’s called the triad in the clinical encounter and some of the challenges that come with that,” she says. “You have a caregiver, a patient and a clinician.”
Older patients may have grown up with a paternalistic model, where whatever the doctor says is what must be done, Bylund adds.
Bylund and her colleagues developed models to help caregivers communicate more effectively with doctors. One, called PACES, encourages caregivers and patients to present information, ask questions, check understanding, express concerns and state preferences. Caregivers may need to use some additional communication skills — for example, introducing themselves to the doctor, asking permission from the patient to share information and checking with their patient to make sure what they’re saying is accurate. These conversations help build trust between caregivers and their loved ones and between doctors and caregivers.
Take Care of Yourself
Managing clinical conversations and constantly sharing information about a loved one’s condition with friends and family can take a toll on caregivers. Also exhausting: feeling as though they never get a break. Yet many caregivers struggle with the balance of finding the resources they need to make sure their loved one is cared for and feeling guilty when they need a pause.
“Taking care of yourself is one of the most important things that should be on every caregiver’s list, as hard and impossible as it may seem,” Hlafter says, “even if it’s just arranging for someone to have a cup of tea with your loved one while you run out to do something for yourself.”
Cassidy agrees, adding that in addition to offering peer support and mentorship, organizations such as Cancer Hope Network can connect caregivers with other resources to ward off burnout. Some of these resources can help with finding respite care or financial assistance. “Financial toxicity is a massive challenge people face,” she says. “All of a sudden you’ve got these additional burdens at home while you’re trying to keep the job that may be providing the insurance that’s getting your loved one treatment.”
Cassidy encourages caregivers to talk with their treatment center’s navigator or social worker. “They know a lot of resources available in your community,” she says. “It’s a great place to start.”
Talking with others who’ve been in the caregiving role can provide reassurance that feeling overwhelmed, exhausted and afraid is normal. Another critical task in avoiding burnout? Try to find personal meaning in the caregiver role.
“Caregiving is one of life’s great honors,” Cassidy says. “You’re fighting alongside somebody you love. It’s also frustrating. Those two feelings aren’t mutually exclusive.”
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.