Publication
Article
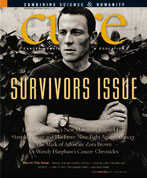
CURE
A Survivor's Map
Author(s):
Paradigm shift finds cancer patients no longer on their own.
In post-treatment America, cancer survivorship is no longer just a pink-ribbon, 5K-run or yellow-wristband state of mind. Survivorship is now a prescription—bearing its own set of guidelines and, finally, its own treatment plan. And now, with more than 10 million cancer survivors in the United States, experts suggest it may soon become its own medical specialty, like podiatry or geriatrics.
This was news, good news, to me when I heard it—a guy who didn’t really know where to turn after nine months of treatment in 2001 for stage 3 colorectal cancer. Sure, I was glad to be off the toxic cocktails, yet I remember feeling a faint sense of loss once my oncologist offered congrats and set me free. I had gained a clean CT (computed tomography) scan, but also had lost a family, of sorts, of caring professionals. I was on my own.
Each year, more than 1.4 million Americans are diagnosed with cancer. Within months hundreds of thousands of them will return to their "normal" lives after treatment, feeling anything but normal and medically underserved, according to the landmark recent report by the Institute of Medicine and National Research Council, "From Cancer Patient to Cancer Survivor: Lost in Transition." Today, optimal survivorship means medical care. It means you’re not quite alone, not merely ticking off a one- or five-year countdown to the next all-clear. The way breast cancer survivor Gretchen Hoag, 45, of Chapel Hill, North Carolina, looks at it, "the perfect survivor isn’t Lance Armstrong. The perfect survivor is you"—meaning her, meaning all of us.
Ellen Stovall, president of the National Coalition for Cancer Survivorship and a 35-year cancer survivor, says that after battling cancer in 1971 and a recurrence 12 years later, her medical record is literally a foot high. “If you took the X-rays alone, they measure 8 inches high,” Stovall says. “Within all those pages are several points of information that are very important in terms of what tests I should be having based on the levels of radiation exposure and the amount of chemotherapy I had.”
Fortunately, these discussions are no longer just concepts at medical meetings. “Cancer survivors coming off treatment really need to be empowered to ask for summaries of their treatment and to ask for a treatment plan,” says Al Marcus, PhD, director of the LIVESTRONG Survivorship Center of Excellence at the University of Colorado Cancer Center in Denver. And the more specific, the better. He likes to see patients carrying notebooks out of their oncologists’ offices, not a mere photocopy of some future appointment. Indeed, a survivorship plan should include: confirmation of diagnosis and hard copies to share with future doctors; a listing of all treatments received; an outline of recommended, coordinated surveillance for both recurrence and new cancer(s); and finally, specific recommendations or tips for nutrition, exercise, intimacy and/or rehabilitation.
Scott Leischow, PhD, professor of family and community medicine and deputy director at the University of Arizona Cancer Center in Tucson, believes survivors will soon see more individually tailored plans, on a disease-by-disease basis, with less mass appeal. That is, he asserts, once survivorship training reaches a tipping point. “I’d like to see every single cancer survivor given a clear menu of options unique to their cancer,” Dr. Leischow says, “because survivorship for someone with lung cancer means something very different than for someone with colon cancer.”
Dr. Leischow’s short-term hope is to find a way to fund patient navigators for each cancer survivor at his medical center. Working with a navigator and toting a prescribed, survivor treatment plan, the patient would then select from a menu that includes: psychological support—one of the most important, yet too often overlooked, resources at a patient’s disposal—as well as drugs and other therapies. Plus, it would direct how these pieces of the plan interact and play out over time. “There would be a plan for the rest of their life,” Dr. Leischow says, including financial and family plans, career goals and an advocate.
Are these hopes, at once, too grand? Or can they be grounded in the real world of oncology practice by, say, next year or the year after? The prescriptions have been written; now it’s up to us, and our doctors, to fill them.
She says the thought of going from doctor to doctor to gather all the information for a treatment summary and follow-up care plan can be overwhelming for a patient. “The average person would never be able to do that,” says Stovall, who served as co-editor of the Institute of Medicine report on survivorship.
But help is on the way. Indeed, in 2006, for the first time ever, the American Society of Clinical Oncology chose “Advocating Survivorship” as part of the theme for its massive annual meeting of almost 30,000 oncologists and other delegates from around the world. And as if to drive the point home, for the third consecutive year, ASCO selected a cancer survivor-oncologist to serve as its president.
A group of healthcare professionals gathered for one of the ASCO sessions to learn the specifics of optimal survivorship from Patricia Ganz, MD, director of UCLA’s LIVESTRONG Cancer Survivorship Center of Excellence and head of the division of cancer prevention and control research at Jonsson Comprehensive Cancer Center in Los Angeles. As chairwoman of the seminar, Dr. Ganz tried to make certain those in attendance understood the significance of the 75-minute session, entitled “How to Write a Survivorship Prescription.”
“Survivors have always had these issues,” Dr. Ganz tells CURE. The point is that the healthcare system is so complicated now and the stress of not knowing how to navigate it is magnified.” Dr. Ganz says survivors receive mixed messages about where they should go and whom they should see for follow-up exams, flu shots and Pap tests after being treated for cancer. With the ever-changing cycle of insurance policies, primary care physicians and specialists, many patients find it tough to keep up with their medical history and long-term follow-up appointments.
“One of the biggest complaints primary care physicians have after they refer a patient to a cancer specialist is that they lose touch with the patient,” said speaker Steven Woolf, MD, a primary care physician at Virginia Commonwealth University, during the session. “In many cases, they never see them again because of lack of communication.”
The seminar outlined a plan where a patient’s oncology team is responsible for connecting with the patient’s primary care physician during and after treatment, with the understanding that after treatment is over, the patient is referred back to the primary care physician. The prescription plan calls for a one-page summary that includes treatment regimens, side effects and a follow-up plan, which is updated over time. “The way I see it, oncologists give a copy to the patient and include one in their chart,” Dr. Ganz says. “The patient has it, and it empowers the patient,” while providing additional information to the primary care physician or future medical team.
A survivorship plan is also more than just a medical history. During treatment, patients may not have had time to attend to their psychosocial needs, but after treatment, doctors can use follow-up appointments as what Dr. Ganz calls “a teachable moment,” referring the patient to counseling, suggesting a smoking cessation program or having the patient meet with a dietitian or physical therapist. “Survivors are our best product in judging success and treatments. If we can’t do a good job after we treat them, we haven’t accomplished anything yet,” Dr. Ganz says.
Although Dr. Ganz was disappointed the ASCO meeting hall wasn’t packed for the survivorship prescription session, she told the physicians in attendance that they were the early adopters, and it was up to them to pass along the survivorship prescription plan to their institutions and colleagues. “Many were anxious to start something,” she says. She was also encouraged to see many advocates and survivors in the crowd. “Patients play an important role. When a patient asks for something, they get it. Increasing the demand makes it not just another piece of paper, but turns it into something useable.”
Dr. Ganz’s colleagues at the event talked about four other queries of interest:
>
What are the optimal techniques for surveillance for recurrence of a patient’s cancer, while keeping close watch on the “rest” of the body?
>
What are the main survivorship issues for each type of cancer? For instance, older patients who receive radiation and/or hormonal treatments for prostate or other cancers may suffer premature osteoporosis and should be treated accordingly.
>
Which post-chemotherapy side effects demand the most vigilance from a survivor’s medical team? Some breast cancer patients who take Herceptin, for example, have an increased risk of heart damage.
>
What is included in a treatment summary and/or survivorship prescription plan?
Survivorship is now a prescription—bearing its own set of guidelines and, finally, its own treatment plan. And now, with more than 10 million cancer survivors in the United States, experts suggest it may soon become its own medical specialty, like podiatry or geriatrics.
Cancer survivors coming off treatment really need to be empowered to ask for summaries of their treatment and to ask for a treatment plan.
At the Perini Family Survivors’ Center at the Dana-Farber Cancer Institute in Boston, these patient “shoulds” or “should-be-tolds” have been in place for more than a year, reports Craig Earle, MD, medical director of the center’s adult survivorship program and a key speaker at the ASCO survivorship seminar. Perhaps surprisingly, however, Dr. Earle says cancer specialists don’t always make the best quarterbacks for long-term, follow-up survivor care.
“Often we think of the medical oncologist as best suited, but survivorship planning is equally important for patients who saw only a surgeon for treatment. The most important thing is that it is clear that someone will take responsibility for each aspect of care, and that everyone knows who that will be.” Sometimes, Dr. Earle says, it may be a general practitioner; other times, an internist or a gynecologist might best supervise survivorship.
With grant funding provided in part by the Lance Armstrong Foundation, the Dana-Farber adult survivorship program relies on nurse practitioners to oversee a good bit of survivorship care, in conjunction with the patient’s team of doctors. Nurse practitioners spend time with the patient on a regular basis looking for evidence of fatigue, depression, joint or limb pain or other long-term health problems, such as lymphedema, a common and often painful long-term effect following lymph node removal or damage from radiation. The oncologist then creates a targeted treatment summary and survivorship care plan that the patient has explained by the nurse.