How to Talk to a Care Team About Post-Mastectomy Chest Numbness
Sensations in the chest after a mastectomy matter because they affect safety and quality of life, an expert said.
A change in quality of life often occurs after a mastectomy, an expert said, which could mean a loss of sensation when hugging a loved one.

Many don’t know that chest numbness after mastectomy is an unintentional, yet real, powerful and potentially permanent side effect. Many also don’t know that it’s possible to reverse or mitigate numbness.
Whether you are in active diagnosis, at high risk due to family history or a genetic marker, trying to understand your preventive options or have already been through a mastectomy, here’s what you need to know about post-mastectomy chest numbness and how you can talk to your care team about it.
How Post-Mastectomy Chest Numbness Happens
Sensation in our bodies is made possible by nerves. Like a wiring system, nerves run throughout our entire bodies and send signals to the brain that allow us to feel touch, temperature and pain. When nerves are cut — a common part of surgery — the connection between that part of the body and the brain is lost, resulting in numbness.
In any type of mastectomy, nerves must be cut to remove the breast tissue. Historically, nothing was done to repair the nerves, and loss of sensation was generally accepted in the surgical and patient communities. But, perspectives are shifting. In 2017, The New York Times published a breakthrough article covering the loss of sensation after mastectomy, giving a voice to many patients and illuminating their deep dissatisfaction with chest numbness. With advances in nerve repair and close collaboration between the breast surgeon and plastic reconstructive surgeon, numbness no longer has to be the accepted norm. We can help minimize the impact to the nerves during the mastectomy (while being oncologically safe) and improve the chances of repair during reconstruction.
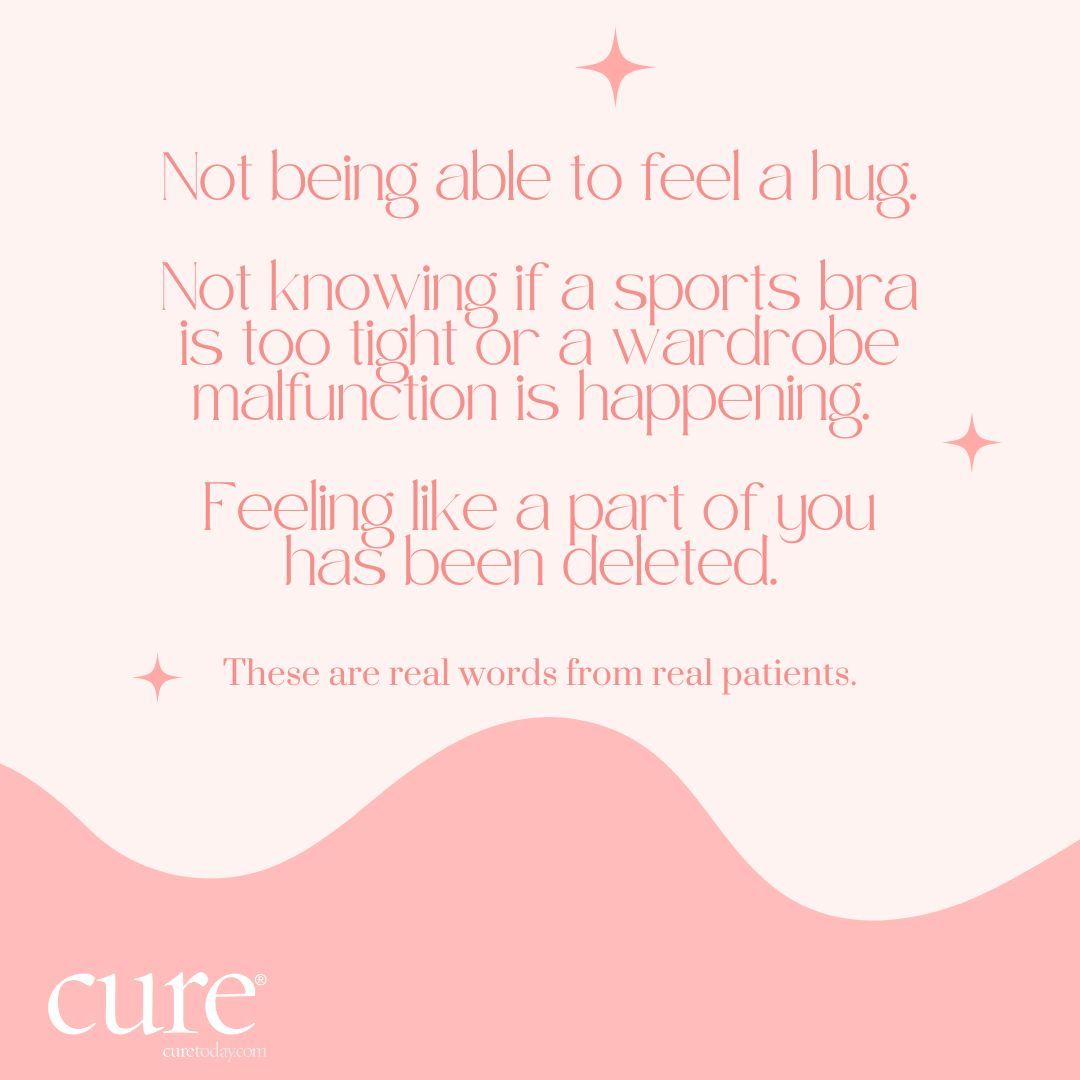
Patients with breast cancer who received mastectomies stated that their quality of life changed when experiencing related chest numbness.
Why Sensation in the Chest Is Important
Feeling in the chest is a factor of both safety and quality of life. Sensation helps us navigate daily situations and helps us feel connected to others.
Safety
Chest numbness affects the ability to feel if the water while showering is too hot, if hot oil splatters while cooking, if you’re getting a sunburn and many other everyday experiences. Household items like heating pads and electric blankets can also pose a potential risk. And, unfortunately, the risks and associated damage aren’t just relevant to the immediate postoperative period but become a part of everyday life.
Quality of Life
Feeling connected to ourselves and to others is essential in how we see our place in the world. Patients have shared that navigating the awkwardness and not being able to figure out their space due to loss of sensation is a truly bizarre feeling. Reconnecting with others again, but this time with a numb chest, can be difficult. The full embrace of a hug is gone. They can’t feel a loved one’s head resting on their heart. These moments of connection have changed.
Patients who have had breast neurotization — the surgical nerve repair technique that can enable sensation to be regained in the chest — say otherwise; some days, they forget about what they went through because numbness isn’t serving as a constant reminder.
Questions to Ask Your Care Team
Breast neurotization is a technique performed during reconstruction and some revision procedures, in which nerves that were cut during mastectomy are repaired and reconnected using a nerve allograft, potentially restoring sensation over time as the nerves heal and grow.
It takes two surgeons to do the job: a breast surgeon and a plastic reconstructive surgeon, both trained in nerve anatomy and breast neurotization. Each surgeon brings a different perspective. As a breast surgeon, I don’t perform neurotization, but what I do while performing the mastectomy sets the foundation.
I talk with my plastic surgeon counterpart about what I’m seeing during the mastectomy and which nerves may be candidates for neurotization so when it’s time for the reconstruction, the plastic surgeon and I have a shared vision based on the patient’s actual anatomy.
Living a Full Life Again
It’s incredibly important to talk with your care team about post-mastectomy chest numbness. A cancer diagnosis or being high risk can bring a lot of emotions, and it can be difficult to think beyond getting the cancer out or taking action to reduce your risk. But feeling like yourself again after mastectomy is also tremendously important. With all the advancements in surgery and treatment options, a lot more is possible in breast cancer care. You deserve the best overall outcome and to feel whole again.
Question & Answer
By talking with both breast and plastic surgeons, you can learn more about your options and what’s possible for you. Here are some questions to ask to start learning more.
Q: What does numbness feel like in a practical sense?
A: Think of the last time your mouth was numbed at the dentist or your foot fell asleep. Now try to imagine that feeling on a larger scale: on your chest. Patients have reported that it can affect their ability to know the physical space they take up. Bumping into door frames, feeling like their breasts are larger than they are or like they’re not part of their body and more can be regular occurrences. Numbness can also affect the ability to feel temperature and pressure as well as cause phantom itch — an itch you can’t scratch because its source doesn’t exist.
While it’s different for everyone, asking your surgeon what numbness might feel like day to day can provide you with a deeper understanding.
Q: Can my nerves regenerate on their own?
A: Some patients might regain some sensation on their own, but this happens spontaneously, and many don’t get feeling back at all. By talking with your care team about nerves — how they work, regeneration and more — you can get the contextual information you need to make an informed decision about what’s best for you.
Q: When is breast neurotization performed?
A: The procedure is done during breast reconstruction surgery (or some revision procedures), which can happen immediately after mastectomy or later on, sometimes even months or years later, and is performed by a plastic reconstructive surgeon with specialized training in microsurgery. Having nerves repaired sooner rather than later typically provides the best outcomes.
When the procedure can take place will depend on what’s best for your treatment plan. Even if you’re planning a delayed reconstruction or a revision procedure, it’s possible that breast neurotization may be an option for you.
Q: How long will it take for sensation to return after neurotization surgery?
A: Having reasonable expectations for regaining sensation is important. Nerves are slow growing, so it can take several months and up to two years to regain sensation after neurotization. Many patients report “zaps” and “tingles” in the months following surgery. These are often good signs, as they mean your nerves are regenerating.
Everybody’s level of sensation is different before surgery and each person’s recovery will vary. Generally, it will not be 100% of what it was before surgery. Your care team can provide more insight based on your case.
Q: Do you have other patients I could talk to and learn more about their experience?
A: Many patients who’ve had the procedure are willing to share their story. Speaking with someone who has experienced chest numbness and has had breast neurotization surgery can provide a real-life perspective that surgeons usually can’t offer.
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.

FDA, Cancer Vaccine Updates and a Misguiding of Breast Cancer Treatment
February 5th 2024One cancer vaccine may still be years away from being available, a breast cancer test may be misguiding treatments for Black women and the review of two oncology regimens are being expedited by the FDA.
Listen