News
Article
Kadcyla Is the ‘First Therapy to Show Improved Survival’ in a Breast Cancer Subset
Author(s):
Kadcyla outperformed Herceptin regarding overall- and invasive disease-free survival in patients with HER2-positive early breast cancer that still had remaining invasive disease after undergoing neoadjuvant therapy.
Kadcyla (ado-trastuzumab emtansine; T-DM1) outperformed Herceptin (trastuzumab) regarding overall survival (OS; time from treatment until death of any cause) and invasive disease-free survival (iDFS; time from treatment until disease worsens) in patients with HER2-positive early breast cancer that still had remaining invasive disease after undergoing neoadjuvant (presurgical) therapy, according to findings from the KATHERINE trial.
“(Kadcyla) is the first therapy to show an improved survival after post-surgical therapy in patients with HER2-positive early breast cancer and residual invasive disease after neoadjuvant therapy,” study author, Dr. Sibylle Loibl, German Breast Group, Neu-Isenburg; Centre for Haematology and Oncology Bethanien, Goethe University, said while presenting the findings at the 2023 San Antonio Breast Cancer Symposium.
The trial initially enrolled 1,486 patients with HER2-positive early breast cancer who received a minimum of six cycles of chemotherapy and a minimum of nine weeks of Herceptin. A second HER2-targeted agent was also permitted.
Within 12 weeks of undergoing surgery, patients were randomly assigned to receive 14 cycles of either Kadcyla or Herceptin. Radiation and endocrine therapy could be administered at the discretion of the investigator, and patients were permitted to switch to Herceptin if Kadcyla became intolerable.
A total of 740 patients were treated with Kadcyla, and 720 were treated with Herceptin. At the 8.4-year follow-up mark, 521 (70.1%) and 461 (62.0%) in the Kadcyla and Herceptin groups, respectively were still alive.
At 8.4 years, fewer patients on Kadcyla experienced invasive disease than those on Herceptin.
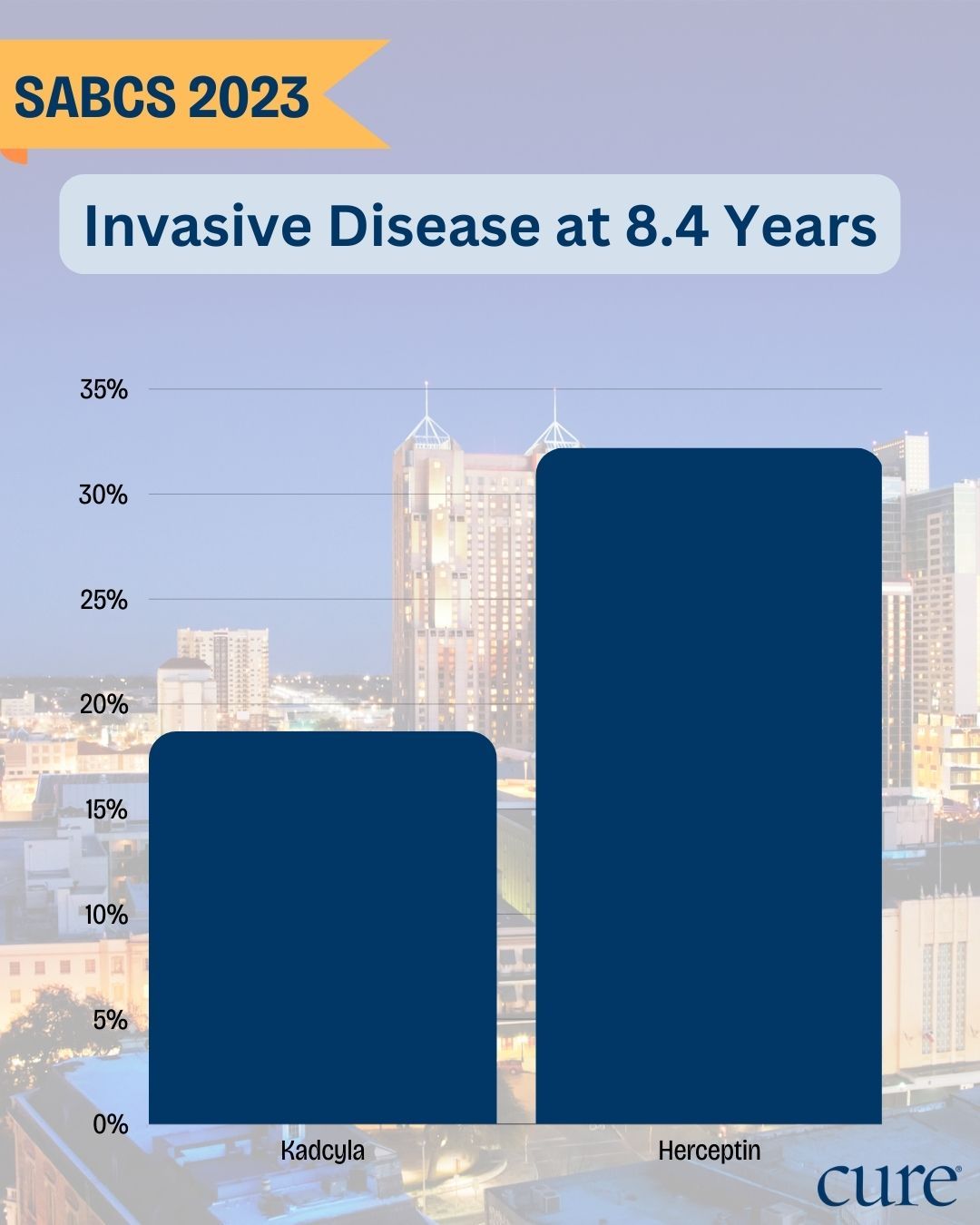
Findings after 8.4 years (101 months) showed that a higher percentage of patients in the Herceptin arm experienced an iDFS event — meaning that they developed invasive disease — compared to those in the Kadcyla arm, at 32.2% (239 patients) and 19.7% (146 patients), respectively. Notably, there was a 13.7% absolute iDFS benefit at seven years.
The most common sites of first iDFS events were:
- Distant recurrence: 21.5% and 14.7% in the Herceptin and Kadcyla cohorts, respectively, including central nervous system (CNS) metastases in 5.1% and 7.0%
- Locoregional recurrence: 6.2% versus 2.2%
- Contralateral breast cancer: 2.6% versus 0.9%
- Death without a prior event: 1.9% in both arms
Most patients went on to receive one or more treatments after experiencing an iDFS event. Most commonly, they were HER2-directed therapies, platinum compounds, taxanes and capecitabine.
These findings further support the promising findings of KATHERINE that were observed years ago.
“Five years back in 2018, the interim analysis for the iDFS was presented at the San Antonio Breast Cancer Symposium (and) demonstrated a large and clinically meaningful and statistically significant benefit for (Kadcyla) over (Herceptin) … At that time, with a short follow-up, overall survival was immature …” Loibl said.
Now, more mature OS data favor Kadcyla at the 8.4-year mark, with a total of 89 patients (12%) experiencing an OS event in the Kadcyla arm, compared with 126 (17%) in the Herceptin arm. Loibl explained that Kadcyla led to an absolute OS benefit of 4.7% at seven years, with a 34% significant reduction in the risk of death.
The causes of death were breast cancer (9.5% in the Kadcyla cohort, versus 15% in the Herceptin cohort; side effects (0.1% versus 0%); and other (2.4% versus 2.5%).
No new safety signals emerged with longer follow-ups from the KATHERINE trial. Twenty-four patients (3.2%) in the Kadcyla group and 12 patients (1.7%) in the Kadcyla and Herceptin cohorts, respectively, experienced any-grade side effects. These included cardiac disorders (0.7% in each arm), nervous system disorders (0.5% versus 0% in the Kadcyla and Herceptin arms, respectively), hepatobiliary disorders (0.3% versus 0%), metabolism and nutrition disorders (0.3% versus 0%), and skin and subcutaneous tissue disorders (0.3% versus 0%).
Serious side effects occurred in 0.3% (two patients) and 0.6% (four patients) of patients in the Kadcyla and Herceptin groups, respectively. They were cardiac disorders (0 vs 0.4%), hepatobiliary disorders (0.3% vs 0%) and vascular disorders (0 vs 0.1%).
Regarding patients discontinuing the study, 105 (14.1%) and 159 (21.4%) in the Kadcyla and Herceptin arms, respectively, stopped treatment with an iDFS even reported, while 117 (15.7%) and 123 (16.6%), respectively, discontinued before an iDFS event.
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.





