- Summer 2008
- Volume 7
- Issue 2
A Better Way to the Brain
New technology and smart drugs take a direct approach to targeting brain tumors.
It started with an odd mix of symptoms: headaches, tunnel vision, a whooshing sound in his ears. But when Chris Funk started having mini-seizures, he headed for the hospital. At 28 years old, Funk was diagnosed with a malignant brain tumor in his left frontal lobe and given a dismal prognosis.
That was 2001. Still alive years later to tell the tale, Funk, of Madison, Wisconsin, credits the talents and persistence of his oncologist for his path to recovery. He points out, however, that the path can be uncertain, for patients and doctors alike. “Even the experts don’t have all the answers.”
Uncertainty is engrained in most studies of the brain, with its intricate wiring and hazy biology. Because the brain is the command center for the entire body, treating cancer in this sensitive organ is tricky. Removing a tumor surgically can damage essential neuronal connections that control mobility, speech, even mood.
Additionally, the biology of the brain is problematic. Between the brain and its blood supply sits a physical barricade called the blood-brain barrier, which restricts the ability of traditional chemotherapy agents to make their way to the tumor. For decades, researchers have sought better ways to fight primary brain tumors without much success. But recent advances have improved prognoses for patients and revitalized research in the area.
“The environment is the most positive I’ve seen in a long time,” says Funk’s oncologist Minesh Mehta, MD, of the University of Wisconsin.
Compared to lung, breast, or prostate cancer, brain tumors are relatively uncommon and occur in a wide range of age groups. This year, more than 21,000 American adults will be diagnosed with a primary malignant brain tumor, according to the American Cancer Society. (Benign brain tumors make up about 22,000 additional diagnoses.) Due in part to their rarity, funding for research into the area has been kept comparatively low, and investigators face plenty of additional challenges.
Brain tumors are actually a collection of different tumor types. From benign meningiomas that might never require surgery to malignant glioblastomas, each has its own unique properties and ideal treatment strategies.
As in Funk’s case, brain tumors often present as seizures or unrelenting, progressive headaches, though the symptoms and effects vary depending on the tumor location. If it lies within a functional area of the brain, problems in speech, vision, or mobility might occur.
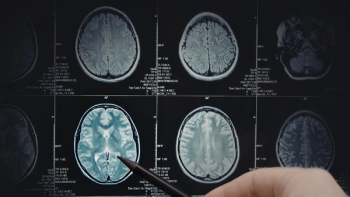
Brain tumors are most often identified with an MRI (magnetic resonance imaging) scan, which picks up on masses, swelling, increased cell density, and leaks in the blood-brain barrier. Biopsy and additional MRI tests determine the type and location of the tumor.
For benign brain tumors, surgery is often successful at fully removing the tumor. Surgery is also used whenever possible for malignant tumors. Although rarely curative in these cases, surgery can improve a patient’s quality of life by relieving symptoms, such as headaches and seizures. But the surgery itself poses significant risks, as brain function may be damaged in the process.
“In the brain, nothing is redundant,” says Dr. Mehta. “So removing a chunk of it risks causing a deficit.”
To limit the potential for problems, doctors are now relying on a high-quality map of the brain and enhanced views of the tumor within it. “Instead of just hoping for patients to come out intact, with fancy imaging studies, we can see critical structure and functional areas of the brain and plan the surgery accordingly,” says Dr. Mehta.
“Preoperative tests let us estimate the risk of surgery, to tell if it’s feasible to do a gross total resection,” says neurosurgeon Michael Vogelbaum, MD, PhD, associate director of the Brain Tumor and Neuro-Oncology Center at the Cleveland Clinic. When important brain structures lie near the tumor, surgeons remove only what they can without damaging key neurons.
The biggest change in the last 20 years has been in the marriage of radiology and imaging into the operating room.
Susan Chang, MD, says that in her neurosurgery department at the University of California, San Francisco, attempts are being made to design MRI machines that use stronger magnets, which afford greater detail. An advanced version, called functional MRI, associates certain areas of the brain with particular activities.
At age 23, Jonathan Woodruff, of Miller Place, New York, underwent such a procedure just before his high-grade tumor was removed in 2003. “It was like a regular MRI,” Woodruff recalls, “except they told me to move different fingers, wiggle my toes, and speak, while they mapped out my brain.”
“The areas involved light up on the [functional] MRI,” says Dr. Vogelbaum, “and then we can look at the relationship of those spots to the location of the tumor.” Language deficits can also be avoided if the surgeon wakes the patient during surgery to speak while the tumor is removed. If problems surface, the surgeon changes tactics to prevent long-term speech defects.
Imaging can also be done during the resection surgery, using a fully integrated operating room plus MRI combination, such as BrainSUITE, to help navigate the brain and determine how much of the tumor remains.
“The biggest change in the last 20 years has been in the marriage of radiology and imaging into the operating room,” says Henry Brem, MD, director of neurosurgery at Johns Hopkins Hospital in Baltimore. “We have made tremendous advances in imaging and computer navigation systems that allow us to localize tumors by fusing the imaging data to the procedure we’re doing. Therefore, the ability to remove the tumors safely has radically improved.”
In the future, the goal will be to perform surgery without even opening the skull, says Keith Black, MD, director of the Maxine Dunitz Neurosurgical Institute at Cedars-Sinai Medical Center in Los Angeles. “We’re looking towards a new paradigm of surgery now—noninvasive ways to eliminate these tumors, like focused microwave imaging, where we put in a small microwave probe into the tumor without doing a big operation.”
Computer assistance is also improving radiation therapy, most often used to treat patients with highgrade tumors. Because of radiation’s side effects, including fatigue, hair loss, and memory loss, and the lack of a clear survival advantage, there is some debate over whether radiation should be used to treat less aggressive brain tumors.
Radiation can be effective following surgery, and even later should the tumor recur, as happened to Funk. Four years after the bulk of his tumor was removed, Funk again experienced seizures. The tumor now spanned both hemispheres of his brain, making surgery implausible.
Funk was referred to Dr. Mehta, who suggested six weeks of traditional whole-brain radiation. Two years later, Funk is doing well, taking anti-seizure medications and practicing yoga, although he says his memory isn’t what it used to be. “Books I’ve read and movies I’ve seen aren’t as easily recalled,” says Funk, who formed the nonprofit
To limit side effects, radiation oncologists are trying to skillfully focus the radiation beam so that it avoids normal tissue. Improved accuracy is provided by a process called image-guided radiation therapy, which uses a computer to reproducibly position the patient—and the tumor—from one day to the next. A smaller, more focused radiation beam can then be used. Intensity-modulated radiation therapy, an advanced type of conformal (precise) radiation therapy, uses multiple beams with varying intensity to treat the tumor.
Radiation is also being used with stereotactic radiosurgery. Gamma Knife, for example, uses a computer to simultaneously focus about 200 small beams onto a tumor. The treatment is usually done once, and the patient’s skull must be anchored to a specialized helmet to maintain positioning during the procedure. Not only uncomfortable, the helmet attachment can cause complications, such as infection.
A similar technique, known as CyberKnife, bypasses the need for the helmet by instead using real-time imaging to make adjustments. Gamma Knife is used for small- to medium-sized tumors, while CyberKnife is typically employed for large lesions.
In addition to surgery and radiation, chemotherapy is now often used to treat aggressive tumors and has resulted in improved survival and quality of life for some patients. The Food and Drug Administration has so far approved two chemotherapies for treating brain tumors—Temodar (temozolomide) and Gliadel wafer.
Approved in 1999 for refractory anaplastic astrocytoma and in 2005 in combination with radiation for new diagnosed glioblastoma multiforme, Temodar damages DNA and is thereby toxic to rapidly dividing tumor cells. Common side effects include nausea, fatigue, and headaches. Funk received Temodar, administered as an oral pill, after his surgery in 2001.
Gliadel wafer, on the other hand, is a challenge to administer and requires an expert surgeon. Immediately following tumor resection, the surgeon places wafers made of a biodegradable polymer inside the resulting cavity in the brain. The wafers contain a cytotoxic agent called BCNU (carmustine) and over the following weeks, the agent leaks out into the nearby brain tissue, killing tumor cells that escaped surgical removal. The FDA first approved Gliadel wafers in 1996 for recurrent glioblastoma multiforme and in 2003 for newly diagnosed high-grade malignant gliomas.
For Woodruff, the drug was part of a program that saved his life. Doctors implanted wafers after removing three-quarters of his right frontal lobe to resect the tumor. The wafer can cause infection, seizures, or vomiting, but the side effect Woodruff recalls most is disorientation. “But you know what, I’m still alive. So whatever they did worked.” He’s had no indications of recurrence.
Neurologists continue to search for more chemotherapy options. “The biggest difficulty in treating malignancies is in the delivery,” says Dr. Vogelbaum. In other organs, blood vessels that feed the area are leaky and allow systemic drugs to seep out passively into the surrounding tissue. The brain, however, has a more stringent border patrol—the blood-brain barrier.
“The brain blood vessels essentially form a wall,” says Dr. Black. “They do not allow anything to get out. So most chemotherapeutic agents do not get to the brain.” To pass the barrier, therapeutic compounds must either dissolve through the lipid cell membrane, as Temodar does, or be selectively carried across or placed, as with the Gliadel wafer.
A technique in clinical trials, known as convection-enhanced delivery, aims to bypass the barrier mechanically. In this method, catheters are inserted into the brain during surgery. Chemotherapeutics are then slowly pumped in to treat the tumor locally. Not all surgeons are a fan of this approach, however. “It’s a bit crude,” says Dr. Black. “It’s certainly not the most ideal way of doing things.”
If we have the tissue of the tumor, we can say this pathway or that is affected, and then we can pick the ideal drugs for that patient.
A number of cancers have been successfully treated with a class of drugs called angiogenesis inhibitors, which may offer hope for brain tumor patients as well. Avastin, already approved for colorectal, lung, and breast cancers, as well as a new experimental agent called cilengitide do not need to pass through the blood-brain barrier to reach the tumor. Rather, because the agents work by blocking the growth of blood vessels to the tumor, the subsequent cutoff of oxygen and nutrients to the tumor causes it to shrink.
Both agents had some success in phase II trials, but serious side effects, such as internal bleeding, can occur. Common side effects of angiogenesis inhibitors include fatigue, nausea, and diarrhea. Avastin can also cause high blood pressure, which can be managed with medication. Genentech, the maker of Avastin, plans to submit the drug for approval later this year for relapsed glioblastoma multiforme.
In the future, a genetically altered virus called Delta-24-RGD may kill off brain tumor cells that are most resistant to radiation and chemotherapy. The virus is modified so that it infects and kills only tumor cells, leaving normal brain tissue unharmed. Although not yet in clinical testing for brain tumors, Delta-24-RGD was recently shown to nearly double survival times in mice that were grafted with highly malignant human glioblastoma cells.
These and many other agents hold promise, but the best strategy may lie in mixing and matching. “In the future, combinations of drugs are going to be very powerful,” says Dr. Brem. “Every other cancer is treated with multiple agents, and we’re finding that certain drugs work best in combination with each other.”
For this approach to be most fruitful, each patient’s tumor should be considered a unique case, says Dr. Chang. “If we have the tissue of the tumor, we can say this pathway or that is affected, and then we can pick the ideal drugs for that patient.”
Considering the complexities of the brain, patients should seek out centers that have the best equipment and staff to handle the charge.
“There are 3,000 neurosurgeons in the country,” says Dr. Black, “but really only a couple hundred specialize in brain tumors. More than technology, experience will ensure a much better operation. The idea is to be like a thief in the night—sneak in, get the tumor, and sneak out without the brain ever realizing that we’ve been there.”
Dr. Brem says that given the range of new options, “it’s vital that patients be treated in centers that have access to experimental trials and the newest treatments, and that it’s individualized to the patients. It’s not a standard one-size-fits-all therapy.”
Dr. Vogelbaum agrees. “Our attitude here [at the Cleveland Clinic], and at other places like this, is that we consider investigational therapies in this disease to be part of our standard regimen, because there is no cure. At some point, these patients will need something more.”
Articles in this issue
over 15 years ago
On a Rollover 15 years ago
Detection Toolsover 15 years ago
Federal Laws Against Employer Discriminationover 15 years ago
Understanding Hereditary Cancerover 15 years ago
A Difficult Inheritanceover 15 years ago
Healing Escapesalmost 17 years ago
Web Exclusive: Another Sonalmost 17 years ago
Web Exclusive: Saving Livesover 17 years ago
Breaking News from ASCOover 17 years ago
The Diagnosis Dilemma