Discussing Goals of Treatment With Patients and Caregivers
Episodes in this series
Priscilla Brastianos, MD: How do you discuss these goals with patients and their caregivers, and what challenges do you have when you’re presenting these issues to patients and their caregivers?
Raymond Sawaya, MD: Patients are not experts in the field, so our job is to explain the options that are available to them. Fortunately, there are many options available to patients when they are diagnosed or found to have brain metastasis. Our role is to provide the information in a clear way and to help them make a decision. Sometimes the decision is not obvious, so we need to lay out the pros and cons of each treatment.
Vinai Gondi, MD: It’s an assessment of what their current situation is doing. Katie Doble’s is a good example of an unfortunate situation where she presented acutely symptomatic, with a lesion in a tough spot in the brain, the pons. What her team did is exactly what we do—get her in, get her treated, shrink it down, hopefully reverse the symptoms and maintain her quality of life as much as possible. To some extent,we take situations like Ivy Elkins’ situation, where she was not having any symptoms. In that case, we had room to think about alternative options to maintain her quality of life and use drug therapy. It’s understanding how patients are presenting, understanding the type of systemic cancer that they have, the type of systemic therapies available off trial and on trial, and then complementing all that information with what we know can work with focal therapies to the brain, including radiotherapeutic and surgical options.
Priscilla Brastianos, MD: Adding to that, it’s taking what the goals and the needs are for that particular patient, whether it’s quality of life or wanting to go on to a clinical trial. Putting out what we have to offer but also combining that with what the patient hopes for. Dr Ahluwalia, can you tell us a little more about some of the issues you confront when treating brain metastases—the challenges—and speak a little to the blood-brain barrier?
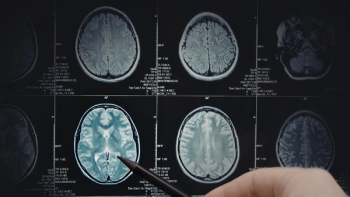
Manmeet Ahluwalia, MD: As we all know, treating brain metastases is a complex issue. As Dr Gondi alluded to, you have a two-compartment disease. When someone has brain metastases, often they’ll have a systemic cancer as well, which is ongoing. With the brain, we have an additional challenge that our traditional chemotherapies do not cross this lining around the brain called the blood-brain barrier. A lot of these patients, when they were treated with the traditional chemotherapies, had response rates of benefit in less than 5% of the cases. In the past, these patients were mostly handled by our neurosurgical colleagues or our radiation oncology colleagues, who either operated on these patients or delivered some form of radiation. It used to be whole-brain radiation and more focused forms of radiation, as has been described in the cases before.
In the last decade or so, a lot of drug development has taken place, and we are in the era of precision medicine. We’re in the era of immunotherapy. Really exciting times as physicians, but more important for patients, because a number of these therapies can penetrate the blood-brain barrier, especially the small-molecule tyrosine kinase inhibitors, as Ivy described to us that she was treated on. She had eight brain metastases, which very nicely disappeared. In her case, she got a complete response with use of these small-molecule tyrosine kinase inhibitors.
Overall, I would like to highlight that whenever someone has brain metastases, as Dr. Gondi alluded to, we need to take into account whether patients are symptomatic or asymptomatic and what the goals of care are—keep patients and their caregivers central to the discussion. Involve them in picking the choices they would like, depending on what their goals are for themselves, and then picking the therapy that will have the least toxicity profile and the best chances of outcome. But a lot of times this is managed in a multidisciplinary manner using tumor boards, where we all deliberate and say, “What’s the right choice for this patient?”—whether it’s just a targeted therapy by itself, a combination of a focused form of radiation with targeted therapy or using immunotherapies that are showing benefit in the brain. Every patient is unique, and individualized care in a multidisciplinary manner—keeping the patients and the caregivers central to the discussion—is the key way to move forward.
Transcript Edited for Clarity