Discussing the Potential for Brain Metastases With Patients
Episodes in this series
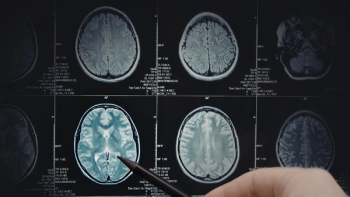
Priscilla Brastianos, MD: At what point do you discuss the potential for brain metastases with patients, given that we know that the incidence is rising and we know how common brain metastases are in certain histologies?
Manmeet Ahluwalia, MD: Great question. For someone with stage IV lung cancer, you have to talk about brain metastases often from the outset, because 20% or 25% of these patients may have brain metastases even at diagnosis, and NCCN [National Comprehensive Cancer Network] recommends an MRI screening for these patients. For example, we know patients with hormone-positive breast cancer have less likelihood of developing brain metastases. But those who have triple-negative disease or who have HER2+ [human epidermal growth factor receptor 2-positive] disease may have a greater propensity. If someone has a stage IV breast cancer, their chances of having brain metastases is around 9% to 12% based on a recent review from Boston that looked at the SEER [Surveillance, Epidemiology, and End Result Program] data. It might be reasonable to alert such patients to be looking out for neurological symptoms they may encounter. If someone has brain metastases, we are able to find out sooner because we know we are able to manage those brain metastases, if someone has a limited number of brain metastases, better compared with someone who has a number of brain metastases.
Priscilla Brastianos, MD: The same goes for patients with advanced melanoma to a metastatic melanoma, where about 50% of those patients develop brain metastases too. It’s really important for patients to be aware that this is a possibility and that if they do develop neurological symptoms, they should let their physician know fairly early. At what point do you discuss clinical trial enrollment with patients?
Manmeet Ahluwalia, MD: As oncologists who are involved with clinical investigations, we know that trials are the way to move the field forward. We like to bring up trial discussion at the very onset if someone is diagnosed. We always try to look if there’s a clinical trial for such patients because a lot of times management of brain metastases is a multidisciplinary effort, and we want to make sure we are providing the best care to our patients. In the past, most of the clinical trials excluded patients with brain metastases. However, several of us who have been involved in the field and who have been leading in this aspect have worked hard to get trials that primarily focus on brain metastases. Every time someone has a brain metastases, we screen through a portfolio to see if there’s a clinical trial for those patients. We like to talk about it because if we do not have a trial and maybe you have a trial, we are always happy to refer, because these patients with brain metastases are those who have complex cancer, and we always feel a complex cancer should be managed at a tertiary care center, a place that has access to clinical trials while providing best possible care or maximum potential…for such patients.
Priscilla Brastianos, MD: I completely agree. And in the current era, there are more clinical trials for patients with brain metastases. As you said, in the past, there were very few. Encouraging patients to enroll in clinical trials when they’re feasible is a good idea. Final question for you, Dr. Ahluwalia, do you usually meet with patients and caregivers together to discuss these things? Who else in your office participates or manages these discussions?
Manmeet Ahluwalia, MD: We like to meet with the patient and the caregiver together, because when someone has a diagnosis of cancer, it becomes a family perspective. A patient, specifically when they have brain metastases, may have neurological symptoms, and at that time their needs substantially increase depending on how symptomatic they are. The caregiver’s role is of immense importance in such patients. We like to understand what the patient’s situation at home is and who is going to take care of them. We like to talk about potential risk for seizures and potential risk for falls. And we like to make sure that the patient and their family, which includes caregivers or friends who are going to be involved in the care of the patient, are actively involved in that discussion.
When we manage patients with brain metastases, we like to take care of such patients in a multidisciplinary manner. We like to talk to the neurosurgeons, our radiation oncology colleagues, medical neuro-oncology colleagues, to pick the best modality to give these patients. I would highlight the role of our nurses, who are going to be extremely important because they interact with these patients most of the time and they’re the first to take the phone call. They’re an important link in the chain of communication. We also like our patients to meet social workers. We like to even see if these patients are willing to undergo neurocognitive battery, so we need research nurses and coordinators for that aspect. There are a lot of people who are involved in the care of these patients.
Then we like to give them support group information, organizations like ABTA [American Brain Tumor Association], NBTS [National Brain Tumor Society], organizations which support patients with brain metastases. Several systemic cancers also have foundations, such as Susan G. Komen and several other foundations, which can help such patients. We like to offer that. A lot of times at our place, either a nurse or a social worker will meet with the patients and caregivers to provide them this information.
Transcript Edited for Clarity