Drug Duo Continues to Show Promise in Advanced Kidney Cancer
Long-term follow-up data showed that Lenvima plus Keytruda continued to show benefit in patients with metastatic kidney cancer.
Lenvima (lenvatinib) plus Keytruda (pembrolizumab) continued to benefit patients with metastatic renal cell carcinoma (RCC), including patients who did not previously receive treatment with an immune checkpoint inhibitor, according to long-term follow-up from a clinical trial presented during the 2023 Kidney Cancer Research Summit.
Lenvima plus Keytruda continued to elicit benefit in patients with advanced kidney cancer.
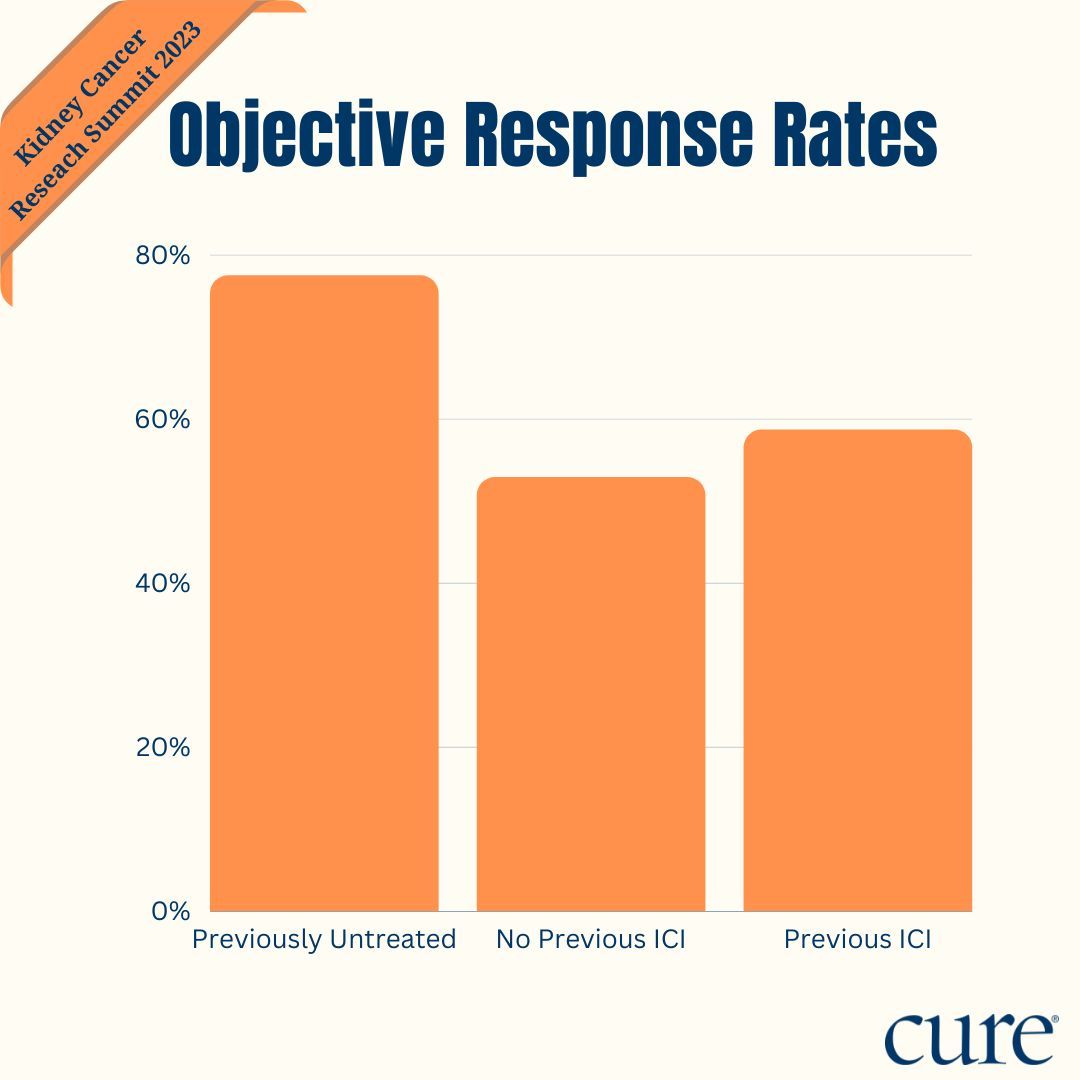
Twenty-two treatment-naïve patients achieved an objective response rate (ORR; meaning that they experienced their tumor shrink or disappear) of 77.5% compared with 52.9% in previously treated, immune checkpoint inhibitor (ICI)–naïve patients (17 patients) and 58.7% in ICI-pretreated patients (104 patients). The median duration of response (DOR) was 24.2 months, nine months and 14.1 months, respectively.
When responders were evaluated by response duration, 58.8%, 33.3% and 34.4% of treatment-naïve, previously treated ICI-naïve, and ICI-pretreated patients had responses lasting at least 18 months. For 24 or more months, these rates were 47.1%, 22.2% and 24.6%, respectively, and for at least 30 months, these rates were 41.2%, 22.2% and 8.2%, respectively.
“The responses remained durable in a subset of patients who were previously treated but ICI naïve, but also in patients who received ICIs as prior systemic therapy,” Dr. Chung-Han Lee, an assistant attending physician at Memorial Sloan Kettering Cancer Center, said in a presentation during the meeting.
The combination of Lenvima and Keytruda is FDA approved as a first-line treatment for patients with advanced RCC, based on findings from the phase 3 CLEAR trial (Study 307/KEYNOTE-581). In the study, the drug duo led to statistically significant and clinically meaningful improvements in progression-free survival (PFS; time from treatment until death or disease worsening), overall survival (OS; time from treatment until death of any cause) and ORR compared with Sutent (sunitinib).
In the RCC cohort of the phase 1b/2 Study 111/KN146 trial, which evaluated the regimen across various solid tumors, efficacy data with the combination were stratified based on whether patients were treatment naïve, previously treated and ICI naïve, or ICI pretreated. Patients were given oral Lenvima at 20 mg daily and 200 mg of intravenous Keytruda every three weeks.
To be eligible for enrollment for the RCC cohort, patients had to have metastatic clear cell RCC with measurable disease and have received zero to two prior lines of anticancer therapy or with an ICI. The primary end point was 24-week ORR, and secondary end points were ORR, DOR, PFS, OS and safety/tolerability.
At the primary analysis, 145 patients had been enrolled on the trial and 143 were evaluable for efficacy analyses. The ORR at 24 weeks was 72.7% in treatment-naïve patients (16 of 22 patients), 41.2% in previously treated, ICI-naïve patients (seven of 17 patients) and 55.8% for ICI-pretreated patients (58 of 104 patients).
At the 2023 KCRS, Lee unveiled the final findings from the RCC cohort, which includes an additional two years of follow-up and a database lock date of Aug. 24, 2022.
Regarding baseline characteristics, in the treatment-naïve cohort, the median age was 55 years (range, 42-83), most patients were male (82%), and 41% of patients had an ECOG performance status of 1, meaning that they could perform their daily tasks with little to no impact due to their disease.
Patients had favorable- (41%), intermediate- (45%), or poor-risk disease (14%) via the Memorial Sloan Kettering Cancer Center prognostic risk group; these were similar percentages when determined via International Metastatic RCC Database Consortium (IMDC) prognostic risk criteria. PD-L1 combined positive score (CPS) was 1 or higher in 55%, less than 1 in 41%, and not available in 5% of patients. Eighty-two percent of patients underwent prior nephrectomy and half of patients each had 1 or 2 or more metastatic sites.
In the previously treated, ICI-naïve cohort, the median age was 66 years (range, 52-76), 76% of patients were male and also had an ECOG performance status of 1. Patients had either favorable- (53%), intermediate- (35%), or poor-risk disease (12%) via the MSKCC prognostic risk group; via IMDC prognostic risk criteria, these rates were 29%, 59%, and 12%, respectively. PD-L1 CPS was one or more in 41%, less than one in 47%, and not available in 12% of patients. All patients underwent prior nephrectomy (particle or full surgical removal of the kidney) and 6%, 41%, and 53% of patients had zero, one or two or more metastatic sites, respectively.
Finally, in the ICI-pretreated group, the median age was 60% (range, 36-82), 77% of patients were male, and more than half (55%) had an ECOG performance status of 1. Patients had either favorable- (36%), intermediate- (42%), or poor-risk disease (22%) via the MSKCC prognostic risk group; these rates were 17%, 59%, and 25% via IMDC prognostic risk criteria. PD-L1 CPS was 1 or higher in 44%, less than 1 in 43%, and not available in 13% of patients. Seventy-six percent of patients underwent prior nephrectomy and 1%, 17%, and 82% had 0, 1 or 2 or more metastatic sites.
Additional findings showed that, in the ICI-pretreated group, the median time from the last anticancer therapy to the first dose of study drug was approximately 1.5 months with 92% of patients receiving ICI as part of their most recent line of systemic therapy.
“Responses to (Lenvima/Keytruda) were seen regardless of what type of systemic therapy after their last prior therapy,” Lee added.
In regard to PFS, the median PFS in the treatment-naïve group was 22.1 months, 11.8 months in the previously treated, ICI-naïve group, and 11.6 months in the ICI-pretreated group. The 18-month PFS rates were 67.2%, 25.8% and 34.5%, respectively.
Twenty-four–month PFS rates were 48.0%, 21.6% and 23.1%, respectively. Finally, 30-month PFS rates were 33.6%, 14.4% and 19.2%, respectively.
Longer OS data were also assessed. In the treatment-naïve group, the median OS was 55.8 months; the median OS was 30.3 months and 32.1 months in the pretreated ICI-naïve and ICI-pretreated groups, respectively. The 18-month PFS rates were 90.9%, 80.4% and 70.3%, respectively; 24-month PFS rates were 90.9%, 80.4% and 64.2%, respectively. Finally, the 30-month PFS rates were 76.6%, 53.6and 54.4%, respectively.
Regarding safety, no new safety signals were identified with the longer follow-up, Lee noted. “For those who were treatment naïve, the first time to dose reduction with (Lenvima) was 6.5 months. For those who were previously treated […] this was 2.9 months for ICI-naïve patients and 2.1 months for ICI-pretreated patients.”
Grade 3 or higher (moderate to sever) treatment-related side effects were reported in 63.5% of patients in ICI-pretreated patients and in 66.2% of patients overall. In all patients, these included diarrhea (6.9%), fatigue (5.5%), proteinuria (11.0%), hypertension (22.1%), nausea (1.4%), decreased appetite (1.4%) and arthralgia (2.8%).
Clinically significant side effects that were grade 3 or higher (47.6%) in all patients included hypertension (25.5%), proteinuria (11.0%), hemorrhage (3.4%), renal events (4.1%), hepatotoxicity (4.8%), arterial thromboembolic events (3.4%), and cardiac dysfunction (2.1%). Side effects of special interest (13.1%) were adrenal insufficiency (1.4%) and colitis (3.4%).
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.
Kidney Cancer Subtypes, Tumor Stages May Predict Recurrence, Prognosis
January 30th 2024Real-world data demonstrated that knowing a patient’s stage and subtype of renal cell carcinoma, a type of kidney cancer, may provide cancer teams with the information needed to determine potential prognosis and recurrence risk.
Read More