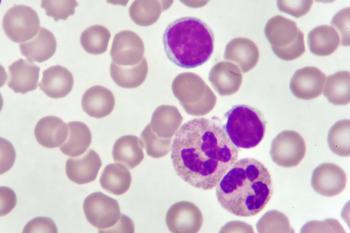
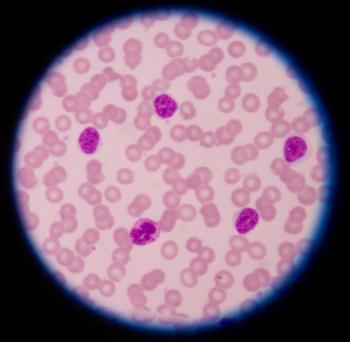
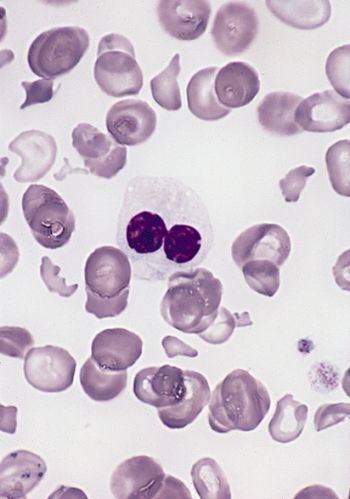
Among patients with relapsed chronic lymphocytic leukemia (CLL) who expressed frequent baseline BTK mutations, responses on the non-covalent BTK inhibitor Jaypirca remained high, according to data presented at the 2023 ASH Annual Meeting.
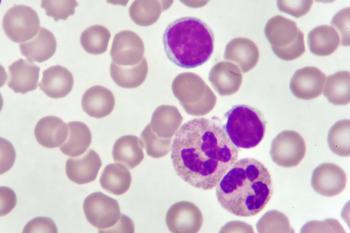
Among patients with relapsed chronic lymphocytic leukemia (CLL) who expressed frequent baseline BTK mutations, responses on the non-covalent BTK inhibitor Jaypirca remained high, according to data presented at the 2023 ASH Annual Meeting.
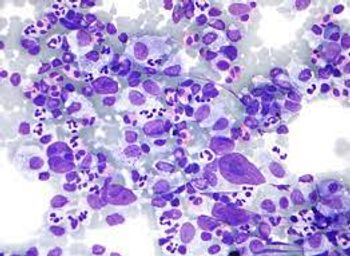
A treatment combination of Sarclisa, Kyprolis, Revlimid and dexamethasone demonstrated a complete response in patients who were newly diagnosed with multiple myeloma.
A comparison of Scemblix (asciminib) and Bosulif (bosutinib) demonstrated greater efficacy and safety/tolerability with asciminib for patients with chronic phase chronic myeloid leukemia.

CURE® recently covered the 2023 American Society of Hematology Annual Meeting. In case you missed it, here is some news that came out of the conference that patients should know about.
Updated safety and subgroup analyses appear consistent with previously reported results from the phase 2 ZUMA-12 study of Yescarta for patients with high-risk large B-cell lymphoma.

Dr. Lucia Masarova sat down with CURE® and discussed the advancements she hopes to see in 2024 for the treatment of patients with myeloproliferative neoplasms.
Children and adults with relapsed/refractory KMT2A rearranged acute leukemia may obtain promising response rates with revumenib, a novel targeted therapy.
Study findings support the use of a financial navigation program, in hopes of aiding patients with multiple myeloma affected by financial toxicity.
A novel cell therapy demonstrated early efficacy and an acceptable safety profile in patients with graft-versus-host disease undergoing haploidentical stem cell transplantation.
Results from an ongoing phase 2 study show the viability for the use of Brukinsa after patients with previously treated B-cell malignancies are deemed intolerant to the next-generation Bruton tyrosine kinase inhibitor Calquence.
Researchers reported long-lasting responses and no new safety concerns in patients with relapsed/refractory follicular lymphoma during the 2023 ASH Annual Meeting and Exposition.

Where a patient lives may affect what kind of treatment they are offered for their CLL or SLL. However, second opinions and learning about one’s cancer diagnosis can help.

The three-year final analysis of efficacy and safety of the REACH3 trial showed that patients with steroid-refractory or dependent chronic graft-versus-host disease benefited more with Jakafi compared with the best available treatment.

Molecular minimal residual disease status may offer clues as to which patients with acute monocytic leukemia will benefit from certain therapies.

Autologous hematopoietic cell transplantation, compared with CAR-T cell therapy, resulted in lower rates of relapse and improved progression-free survival in patients with relapsed large B-cell lymphoma while they were in complete response.

The recent phase 3 TRANSFORM-1 study concluded that navitoclax combined with Jakafi showed significant spleen volume reductions in patients with myelofibrosis.
The stem cell thrapy, Orca-T led to promising relapse-free and overall survival rates in patients with intermediate- to high-risk myelodysplastic syndrome.

Data from the ZUMA-7 trial shows that age alone should not be a barrier of consideration of administering CAR-T cell therapy to patients with large B-cell lymphoma, says Dr. Marie José Kersten.
An artificial intelligence platform was able to tell the difference between patients with prefibrotic primary myelofibrosis and essential thrombocythemia. However, an expert says that there are considerations that patients must remember when it comes to the use of such programs.
The quality-of-life improvement with Abecma in patients with relapsed/refractory multiple myeloma was greater when compared with standard regimens.
Tecartus is safe and effective in real-world patients with relapsed/refractory mantle cell lymphoma, regardless of the presence of high-risk features.

Research demonstrated comparable outcomes in the real-world setting and in the phase 2 MajesTEC-1 trial when it came to treatment with Tecvayli for relapsed or refractory myeloma.

Treatment with an all-oral regimen led to three-year overall survival and relapse-free survival rates of 97% in patients with acute promyelocytic leukemia, a subset of acute myeloid leukemia.
Data demonstrate that iberdomide alone or in combination with other treatments may be a promising option for patients with relapsed/refractory lymphoma.
Adults with graft-versus-host disease who were treated with a three-drug regimen with cyclophosphamide after transplant may have improved survival rate compared with those treated with a two-drug regimen.
Progression-free survival and overall response rates greatly improved in patients with CLL/SLL treated with Brukinsa compared with Imbruvica.
Patients with chronic lymphocytic leukemia tended to switch to another regimen or intensify their Calquence treatment quicker than those given Imbruvica, study results showed.

An expert from the Mayo Clinic explained that the use of a combination of drugs including Darzalex in the first-line setting may lead to better outcomes for patients with multiple myeloma instead of other first-line standard-of-care options.
Treatment with the CAR-T cell therapy ciltacabtagene autoleucel (cilta-cel) led to a 97.9% response rate at two years in patients with relapsed/refractory myeloma in a recent clinical trial.
Two different doses of Venclexta combined with Darzalex and the steroid dexamethasone elicited effective responses appeared safe in patients with t(11;14) relapsed/refractory multiple myeloma.