
Findings from a clinical trial showed that adding Keytruda to neoadjuvant chemotherapy in patients with triple-negative breast cancer significantly improved outcomes and was overall safe and tolerable for patients.

Findings from a clinical trial showed that adding Keytruda to neoadjuvant chemotherapy in patients with triple-negative breast cancer significantly improved outcomes and was overall safe and tolerable for patients.
Treatment with the CAR-T cell therapy ciltacabtagene autoleucel (cilta-cel) led to a 97.9% response rate at two years in patients with relapsed/refractory myeloma in a recent clinical trial.
Two different doses of Venclexta combined with Darzalex and the steroid dexamethasone elicited effective responses appeared safe in patients with t(11;14) relapsed/refractory multiple myeloma.

The addition of a drug commonly used to treat arthritis may reduce the risk of graft-versus-host-disease in patients who underwent haploidentical allogeneic stem cell transplant.

Calquence, a next-generation BTK inhibitor, significantly prolonged survival compared with standard of care, along with no new side effects at three years in chronic lymphocytic leukemia. These findings also pertained to some patients with high-risk genetic features.

The data demonstrated that the combination of Imbruvica and Rituxan conferred superior progression-free survival results in patients with previously untreated chronic lymphocytic leukemia, compared with the chemotherapies fludarabine and cyclophosphamide plus Rituxan.
The use of a novel drug combination yielded positive outcomes in patients with B-cell lymphomas for whom CAR-T cell therapy or stem cell transplant isn’t an option.

Most patients with acute myeloid leukemia and myelodysplastic syndrome achieved strong antibody responses to COVID-19 vaccination, according to recent study results.

Treatment with Ninlaro plus Darzalex and a low dose of the steroid dexamethasone was associated with favorable responses to treatment in non-transplant eligible, intermediate-fit patients with newly diagnosed multiple myeloma.

Patients with chronic lymphocytic leukemia reported improved quality of life when treated with frontline Imbruvica and Rituxan, followed by continuous treatment with Imbruvica.

Patients with relapsed or refractory multiple myeloma experienced a benefit after receiving Xpovio in combination with Darzalex, Velcade and the steroid dexamethasone.

Study results showed that pathologic complete response rates were not significantly different between Black and White patients with high-risk breast cancer, but disparities still exist for other treatment outcomes.

The immunotherapy Kymriah offered similar benefits in patients younger than and older than 18 years with relapsed/refractory B-cell acute lymphoblastic leukemia.

Researchers found that depression and anxiety may skew patient perceptions of participating in blood cancer clinical trials, thus contributing to low enrollment throughout the United States.

Using the presence of minimal residual disease to direct Imbruvica plus Venclexta treatment appears to be a feasible option for patients with relapsed/refractory chronic lymphocytic leukemia.
Recent results demonstrated durable responses and no new side effects for Venclexta plus Imbruvica in pretreated chronic lymphocytic leukemia.

Patients with large B-cell lymphoma tended to have better quality of life that continued to improve over time after receiving Breyzani compared to those given standard of care.

Although patients treated with Lynparza after chemotherapy may experience side effects such as fatigue and nausea/vomiting, these symptoms resolved after treatment was completed in patients with high-risk early breast cancer.
A three-drug regimen was shown to lengthen the amount of time before cancer progressed to the central nervous system — known as central nervous system progression-free survival — in certain patients with breast cancer.
In recent trial results, a dose reduction of Xpovio (selinexor) was associated with longer progression-free survival and duration of response while also reducing side effects in patients with multiple myeloma.

The use of pyrotinib — an experimental drug — plus the chemotherapy capecitabine extended survival compared with Tykerb and capecitabine among patients with pretreated HER2-positive metastatic breast cancer.

Early-phase study results showed that treatment with a novel drug elicits promising outcomes in patients with advanced or metastatic triple-negative breast cancer.

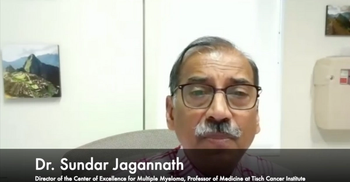
Clinical trial results show that adding Keytruda to chemotherapy prior to surgery for triple-negative breast cancer can improve outcomes and hopefully “increase the chances for patients to be cured,” according to an expert.

The addition of Ibrance to endocrine therapy was not associated with preventing disease recurrence in patients with hormone receptor (HR)–positive, human epidermal growth factor receptor 2 (HER2)–negative early breast cancer, according to final results of the phase 3 PALLAS trial.

Researchers hypothesized that metformin — a medication that helps lower insulin levels in patients with diabetes and is associated with inducing weight loss — might improve breast cancer outcomes.

The use of elacestrant, an investigational therapy, elicited a 30% reduction in the risk of disease progression or death compared with standard of care in a group of patients with estrogen receptor (ER)–positive, HER2-negative metastatic breast cancer.

Ibrance plus Faslodex improved progression-free survival in certain patients with metastatic breast cancer, compared with those who continued to receive an aromatase inhibitor.

Black race is associated with a 3.5-fold increased incidence of lymphedema in women with breast cancer treated with axillary lymph node dissection and radiotherapy, according to recent data.

View the full CURE Educated Patient Breast Cancer Summit Outside of Therapy Session on demand.

View the full CURE Educated Patient Breast Cancer Summit Novel Therapies Session on demand.